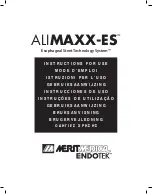
Figure 8.
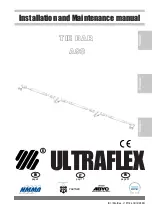
The purse-stringing effect releases the proximal end of
the stent from contact with the esophageal wall, thus
facilitating atraumatic repositioning (Fig. 9).
Figure 9.
In the event that the suture is cut during an attempt to
reposition the stent, the broken strand should be carefully
removed. The stent may be repositioned by applying
gentle traction to the proximal end of the stent using
grasping forceps such as alligator forceps. Open the
forceps and carefully pass the forceps over the proximal
end of the stent at the location of one of the metal stent
connectors as shown in Figure 10.
Figure 10.
One jaw should be positioned outside of the stent,
between the stent and the luminal wall. The other jaw
should be positioned inside the stent. Close the forceps
over the stent connector, grasping as much of the stent
connector as possible. Do not grasp the covering of the
stent alone without grasping the metal stent connector.
Figure 11.
Gently apply traction to the metal stent connector to
reposition the stent proximally (Fig. 11).
WARNING:
Do not attempt repositioning by grasping the
middle or distal end of the stent.
WARNING:
Never use biopsy forceps to reposition the
stent. Only rat tooth grasping forceps may be used to
grasp the suture knot during repositioning. If the suture is
cut, do not use rat tooth forceps to grasp the metal struts
or polyurethane covering to reposition the stent.
WARNING:
Do not rotate the stent using forceps if it is
being repositioned proximally.
REMOVAL OF THE ESOPHAGEAL STENT
The MERIT ENDOTEK™ AL
IMAXX-ES™
Esophageal Stent
design allows for removal of the stent after placement.
The removal of the stent may be necessary in the event
that the stent is not in a desirable location or is improperly
sized. Position the endoscope so that the suture knot at
the proximal end of the stent is visible.
The AL
IMAXX-ES™
Esophageal Stent can be removed
using rat tooth grasping forceps to grasp the suture knot
at the proximal end of the stent and carefully applying
traction (Fig. 8). Do not use biopsy forceps to prevent
cutting the suture. The purse-stringing effect releases
the proximal end of the stent from contact with the
esophageal wall, thus facilitating atraumatic removal (Fig.
9).
In the event that the suture is cut, the preferred method of
stent removal is to utilize a dual-channel endoscope using
two rat tooth grasping forceps. Using both rat tooth
grasping forceps, carefully grasp both the stent cover and
metal struts on oppoite sides of the proximal end of the
stent and apply gentle traction.
In the event the suture is cut and a dual-channel
endoscope is not available, the stent may be removed by
applying gentle traction using rat tooth grasping forceps.
Begin by opening the rat tooth grasping forceps and
carefully passing the forceps over the proximal end of the
stent (Fig. 12). Grasp both the stent cover and metal struts
with the forceps and puncture the cover with the forceps
teeth.
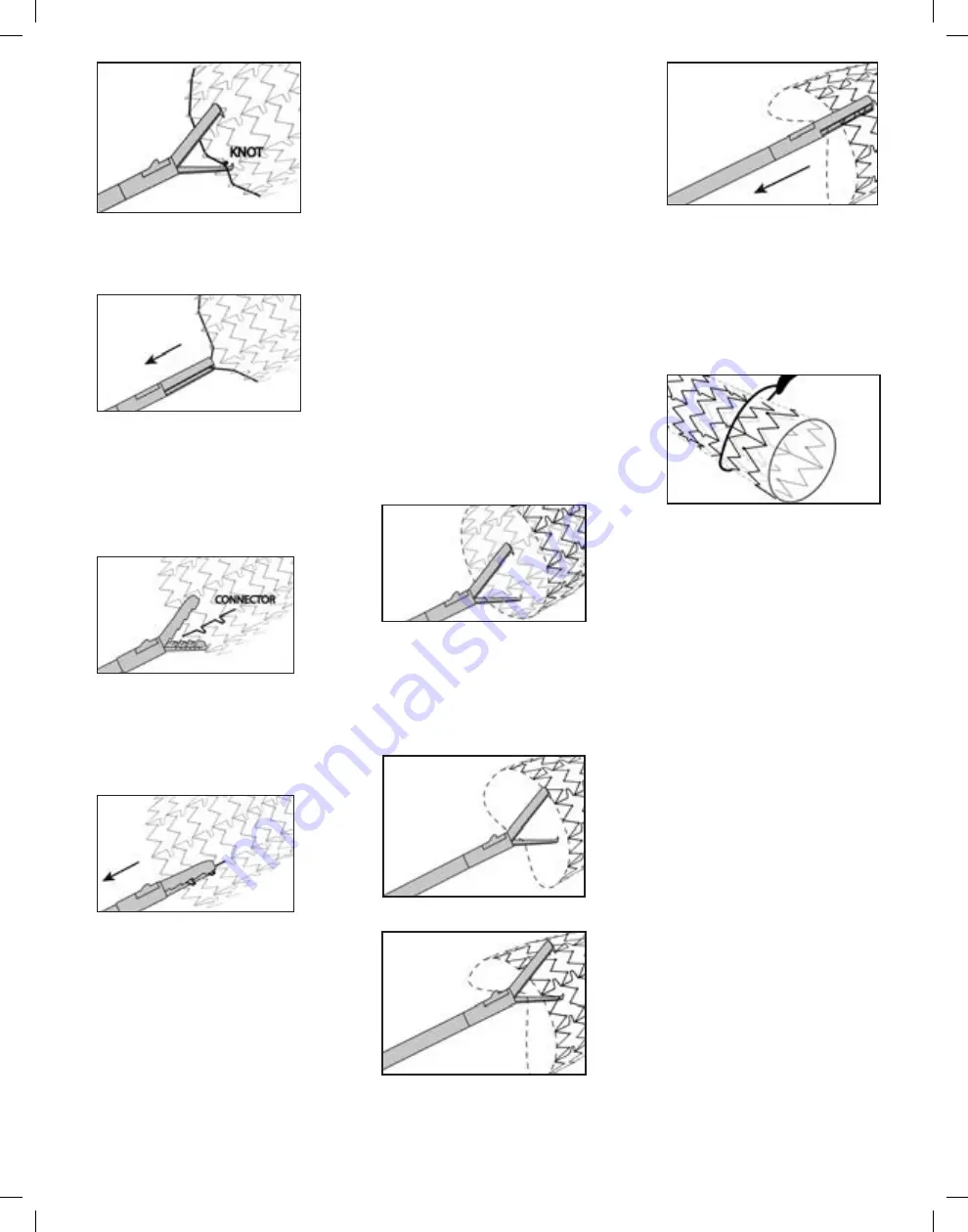
Figure 12.
While keeping the lower forceps tooth hooked in the
stent, open the forceps. Place the upper jaw of the
forceps over the opposite rim of the stent. Grasping both
the stent cover and metal struts with the upper jaw of the
forceps, puncture the cover with the upper forceps tooth.
Close the forceps. Rotate the forceps 1/4 turn and apply
traction to remove the stent proximally (Fig. 13-15).
Figure 13.
Figure 14.
Figure 15.
In the event it is necessary to remove the stent from the
stomach, position the endoscope so that the proximal
end (suture end) of the stent is visible. The ALIMAXX-
ES™ Esophageal Stent can be removed using a snare to
grasp the proximal end of the stent and carefully applying
traction. Open the snare and carefully pass the lasso
around the proximal end of the stent (Fig. 16). Close the
snare and apply gentle traction to remove the stent from
the stomach.
Figure 16.
WARNING:
Do not attempt removal by grasping the
middle or distal end of the stent.
WARNING:
Never use biopsy forceps to remove the stent.
WARNING:
Do not attempt to reload or reconstrain a
deployed or partially deployed self-expanding stent. If it
becomes necessary to remove a partially deployed stent
the entire system should be withdrawn all together. Do
not attempt to advance the outer sheath to recompress
the stent prior to withdrawing the system.
POST-PROCEDURE MANAGEMENT
Patients should have P-A (postero-anterior) and lateral
chest x-rays to record stent position. The patient should be
observed for complications associated with endoscopy,
esophageal dilatation and stent placement. The patient
should be monitored closely for 24 hours post-implant
and should receive only clear liquids during this period.
Patients treated for esophago-respiratory fistula should
receive no fluids or solid food by mouth until after sealing
of the fistula has been confirmed.
Once proper positioning has been confirmed and the
patient has been stabilized for 24 hours, the patient
should be instructed to eat only in an upright position,
avoid certain foods as appropriate, chew food thoroughly
and to take fluids during and following meals.
In order to minimize complications of gastric reflux,
patients with stents in the distal esophagus or across
the gastro-esophageal junction should receive antacid
treatment and should be advised to elevate their head
while supine.
Patients should be scheduled for follow-up examinations
as indicated to confirm proper positioning and stent
patency within 90 days of implant. Patients should be
advised that symptomatic dysphagia following stent
placement could be an indication of tumor impingement
or stent migration and that repeat endoscopy may be
required.